In a report released by the World Health Organization (WHO), the 2023 Global Tuberculosis report paint a picture of substantial global recovery in the expansion of TB diagnosis and treatment services throughout 2022. This positive trajectory signals a commendable reversal of the adverse effects that the COVID-19 pandemic had on Tuberculosis (TB) services.
The report, synthesizing data from 192 countries and territories, reveals a record-high of 7.5 million people diagnosed with TB in 2022, marking the highest figure since WHO initiated global TB monitoring in 1995. The encouraging increase is attributed to the remarkable recovery of health service accessibility and provision in numerous countries.
Notably, countries such as India, Indonesia, and the Philippines, which collectively witnessed over 60% of the global reductions in newly diagnosed Tuberculosis cases in 2020 and 2021, surpassed 2019 levels in 2022, signifying a substantial rebound. This resurgence underscores the resilience of health systems worldwide in the face of unprecedented challenges posed by the pandemic.
Dr. Tedros Adhanom Ghebreyesus, WHO Director-General, expressed optimism, stating, “For millennia, our ancestors suffered and died with tuberculosis, without knowing what it was, what caused it, or how to stop it. Today, we have knowledge and tools they could only have dreamed of. We have political commitment, and we have an opportunity that no generation in the history of humanity has had: the opportunity to write the final chapter in the story of TB.”
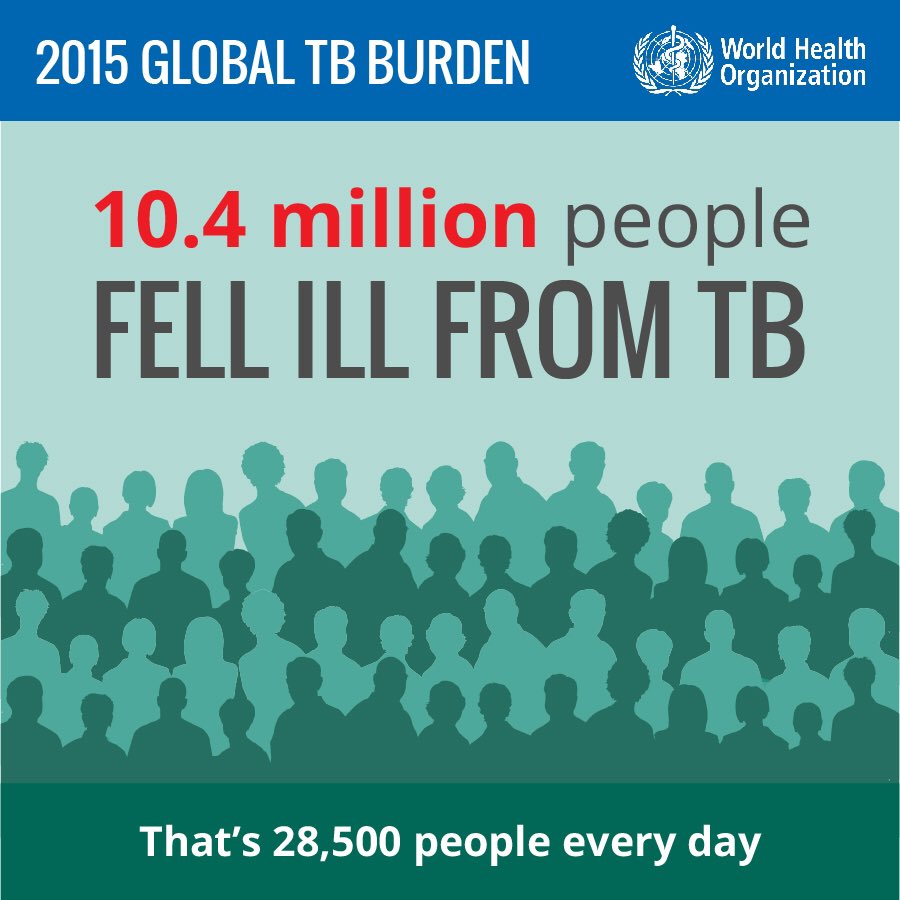
Globally, an estimated 10.6 million people fell ill with TB in 2022, up from 10.3 million in 2021. Geographically, the majority of TB cases were reported in the WHO Regions of South-East Asia (46%), Africa (23%), and the Western Pacific (18%). While these numbers indicate a substantial burden, they also underscore the urgent need for targeted interventions in regions disproportionately affected.
The report notes a decrease in TB-related deaths to 1.3 million in 2022, down from 1.4 million in 2021. However, COVID-19 disruptions in the 2020-2022 period resulted in nearly half a million additional deaths from TB, retaining its status as the leading cause of death among people with HIV. This dual burden emphasizes the intricate intersection of infectious diseases and the challenges posed by the ongoing pandemic.
Multidrug-resistant TB (MDR-TB) remains a significant public health concern, with an estimated 410,000 people developing multidrug-resistant or rifampicin-resistant TB (MDR/RR-TB) in 2022. Alarmingly, only about two in five individuals with MDR-TB accessed treatment, highlighting persistent gaps in addressing the complexities of drug-resistant strains.
While there has been commendable progress in developing new TB diagnostics, drugs, and vaccines, this progress is hampered by the overall level of investment in these areas. A renewed commitment to research and development is crucial to staying ahead of the evolving nature of the TB threat.
Challenges and Targets for 2023-2027 Based on Global Tuberculosis Report:
Despite the positive developments in 2022, the progress was deemed insufficient to meet the global tuberculosis targets set in 2018, with the COVID-19 pandemic and ongoing conflicts contributing significantly to the challenges. Key shortcomings include:
- A 19% net decrease in TB-related deaths from 2015 to 2022, falling short of the WHO End TB Strategy milestone of a 75% reduction by 2025.
- An 8.7% cumulative reduction in the TB incidence rate from 2015 to 2022, far from the WHO End TB Strategy milestone of a 50% reduction by 2025.
- Approximately 50% of tuberculosis patients and their households facing catastrophic costs, far from the WHO End TB Strategy target of zero.
The 2023 UN General Assembly High-Level Meeting on TB has reinforced commitments and set new targets for 2023-2027, including reaching 90% of people in need with TB prevention and care services, using WHO-recommended rapid tests for diagnosis, ensuring the availability of at least one new TB vaccine that is safe and effective, and closing funding gaps for TB implementation and research by 2027.
Dr. Tereza Kasaeva, Director of WHO’s Global tuberculosis Programme, emphasized, “We have strong commitments with concrete targets made by world leaders in the political declaration of the second UN High-Level Meeting on TB, that provides a strong impetus to accelerate the TB response.”
The Global tuberculosis report underscores the importance of collaborative action across health and other sectors to address the social, environmental, and economic determinants of TB. WHO’s Multisectoral Accountability Framework continues to support engagement from sectors beyond health.